Root canal treatment is a dental procedure designed to treat infections within the pulp of a tooth. To ensure the success of this intricate process, accurate diagnosis, and treatment planning are essential. Root canal X-rays play a pivotal role in achieving these goals. In this comprehensive guide, we’ll navigate through the significance, types, and interpretation of X-rays in the context of root canal procedures.
Table of Contents
Understanding the Role of Root Canal X-rays
Root canal X-rays are vital tools for dentists. They provide a clear, detailed view of the areas of your teeth and gums that can’t be seen during a standard dental checkup. Let’s break down how root canal X-rays help in different situations:
Detecting Tooth Infections and Abscesses
- What it does: X-rays reveal infections that have spread to the root of a tooth or the surrounding bone.
- Why it’s important: Infections can lead to abscesses, which are painful pockets of pus. These might not be visible without an X-ray.
- How it helps: By identifying the extent of the infection, the dentist can plan the right treatment, such as a root canal, to save the tooth.
Assessing Tooth Trauma
- What it does: X-rays help assess the damage from tooth injuries like cracks or chips.
- Why it’s important: Some injuries may reach the tooth’s pulp (the soft tissue inside the tooth), which could require a root canal.
- How it helps: X-rays allow the dentist to see the full extent of the trauma and decide the best way to treat it.
Identifying Tooth Decay
- What it does: X-rays detect decay that isn’t visible during a regular dental exam, such as between teeth or under fillings.
- Why it’s important: Hidden decay can worsen if left untreated, leading to more serious dental problems.
- How it helps: Early detection with X-rays enables the dentist to treat decay before it causes further damage.
Evaluating Impacted Teeth
- What it does: X-rays show whether a tooth is impacted, meaning it hasn’t emerged properly and is stuck in the gum or bone.
- Why it’s important: Impacted teeth, like wisdom teeth, can cause pain, infection, or damage to nearby teeth.
- How it helps: The dentist can use X-rays to decide whether to monitor the tooth or remove it.
Monitoring Children’s Permanent Teeth Development
- What it does: X-rays track how children’s permanent teeth are growing and developing.
- Why it’s important: X-rays can identify issues like overcrowding, misalignment, or missing teeth early on.
- How it helps: Early detection allows the dentist to intervene if necessary, preventing bigger problems in the future.
Planning for Extractions, Implants, or Surgeries
- What it does: X-rays give a detailed view of the tooth’s position and the surrounding bone and tissues.
- Why it’s important: This information is crucial for safely planning procedures like tooth extractions, dental implants, or other oral surgeries.
- How it helps: With X-rays, the dentist can plan the procedure accurately, reducing risks and improving outcomes.
Checking for TMJ Problems
- What it does: X-rays help evaluate the temporomandibular joint (TMJ), which connects your jaw to your skull.
- Why it’s important: TMJ issues can cause jaw pain, headaches, and other symptoms, and X-rays can show if there’s arthritis or misalignment.
- How it helps: Understanding the condition of the TMJ helps the dentist create a targeted treatment plan to relieve symptoms.
By providing these crucial insights, root canal X-rays help dentists diagnose problems accurately and choose the best treatments to keep your teeth and gums healthy.
Types of Root Canal X-Rays: Uses, Advantages, and Disadvantages
When it comes to diagnosing and treating root canal issues, X-rays play a crucial role in providing dentists with a clear view of the tooth’s internal structure. There are several types of X-rays used in root canal procedures, each serving a specific purpose. Here’s a closer look at the different types, along with their uses, advantages, and disadvantages.
1. Periapical X-Rays
Uses:
Periapical X-rays are the most common type used during root canal procedures. They focus on capturing the entire tooth, from the crown to the root tip, and the surrounding bone. Dentists use these X-rays to diagnose abscesses, bone loss, and other issues at the root level.
Advantages:
- Provides a detailed image of the tooth and surrounding bone.
- Helps in detecting infections, cysts, and fractures.
- Essential for confirming the success of the root canal treatment.
Disadvantages:
- Limited to a small area, requiring multiple X-rays for comprehensive diagnosis.
- Slight discomfort due to the placement of the X-ray film or sensor in the mouth.
2. Bitewing X-Rays
Uses:
Bitewing X-rays are commonly used to detect cavities between teeth, but they can also provide useful information during root canal procedures. They show the crowns of the upper and lower teeth in a specific section of the mouth.
Advantages:
- Useful for identifying decay and infections in the crown area.
- Provides a good overview of the tooth’s structure above the gum line.
Disadvantages:
- Does not capture the entire tooth, especially the root area.
- Limited use in diagnosing root canal-specific issues.
3. Panoramic X-Rays
Uses:
Panoramic X-rays provide a broad view of the entire mouth, including all the teeth, jaws, and surrounding structures. While not as detailed as periapical X-rays, they are useful for initial assessments and planning complex dental procedures.
Advantages:
- Covers a larger area, offering a complete view of the mouth.
- Helpful in identifying impacted teeth, cysts, tumors, and jaw issues.
Disadvantages:
- Lower resolution compared to periapical X-rays, which may miss small details.
- Not ideal for detailed examination of individual teeth and roots.
4. Cone Beam Computed Tomography (CBCT)
Uses:
CBCT scans provide a 3D image of the tooth and surrounding tissues. This advanced imaging technique is particularly useful for complex root canal cases, such as those involving multiple canals or unusual anatomy.
Advantages:
- Offers a comprehensive 3D view, revealing the tooth’s internal structure in detail.
- Essential for diagnosing difficult-to-detect issues, such as additional canals or root fractures.
- Helps in planning precise treatment strategies.
Disadvantages:
- Higher radiation exposure compared to standard X-rays.
- More expensive and less commonly available than other types of X-rays.
- May require specialized equipment and expertise to interpret the results.
Each type of root canal X-ray has its unique applications, benefits, and limitations. Understanding these differences helps both patients and dental professionals choose the most appropriate imaging technique for accurate diagnosis and successful treatment. Whether it’s the detailed view provided by periapical X-rays or the comprehensive 3D imaging of a CBCT scan, these tools are indispensable in ensuring the best possible outcome for root canal therapy.
Also read: SC Joint X-ray Positioning
When are Root Canal X-rays Recommended?
Root canal X-rays are recommended in various scenarios to provide detailed insights into dental health. Dentists may suggest these X-rays based on specific situations:
1. To Diagnose Tooth Infections:
- When: Persistent tooth pain, swelling, or signs of infection are present.
- Why: Periapical X-rays reveal the extent of infection and help plan root canal treatment.
2. For Assessing Tooth Trauma:
- When: Teeth are injured due to accidents or trauma.
- Why: X-rays help evaluate the extent of damage to the tooth and surrounding structures.
3. Evaluation of Tooth Decay:
- When: Suspected cavities between teeth or in areas not visible during a regular exam.
- Why: Bitewing X-rays reveal hidden cavities and assess overall dental health.
4. Orthodontic Treatment Planning:
- When: Planning for braces or other orthodontic treatments.
- Why: X-rays, including panoramic views, aid in assessing tooth alignment and jaw structure.
5. Impacted Tooth Assessment:
- When: Suspected impacted teeth, especially wisdom teeth.
- Why: Panoramic or CBCT X-rays provide a comprehensive view for surgical planning.
6. Monitoring Dental Development:
- When: Tracking the development of permanent teeth in children.
- Why: Occlusal X-rays help assess the alignment and eruption of new teeth.
7. Before Certain Dental Procedures:
- When: Planning extractions, implants, or other oral surgeries.
- Why: X-rays assist in treatment planning and ensure optimal outcomes.
8. Evaluation of TMJ Issues:
- When: Assessing temporomandibular joint (TMJ) disorders.
- Why: Panoramic or CBCT X-rays help evaluate joint structure and function.
Dentists carefully consider the specific dental concerns and treatment objectives when recommending root canal X-rays. The information gathered from these X-rays is instrumental in accurate diagnosis and planning effective dental care.
The Root Canal X-ray Procedure

Practical Tips on Preparing for a Root Canal X-Ray
Root canal X-rays are a crucial part of the diagnosis and treatment process for various dental issues. Preparing for the X-ray can help ensure a smooth experience and provide the most accurate results. Here’s what you can do to get ready, what to expect during the procedure, and any follow-up care you might need.
1. Before the X-Ray: How to Prepare
- Communicate with Your Dentist:
- Let your dentist know about any medical conditions, allergies, or if you are pregnant. Pregnant patients should inform their dentist, as certain precautions, such as the use of lead aprons, will be necessary to protect the fetus.
- Avoid Eating Right Before the Appointment:
- Some patients, especially those with a strong gag reflex, may find it helpful to avoid eating for a few hours before the X-ray. This can reduce the likelihood of discomfort during the procedure.
- Practice Good Oral Hygiene:
- Brush and floss your teeth thoroughly before the appointment. A clean mouth ensures clearer X-ray images and a more comfortable experience during the procedure.
- Wear Comfortable Clothing:
- Dress in comfortable clothing, especially around the neck and shoulders, as you may need to wear a lead apron during the X-ray. Avoid wearing jewelry, especially necklaces or earrings, that could interfere with the X-ray images.
- Consider Your Comfort Needs:
- If you have a small mouth, gag reflex, or find it difficult to hold still, discuss these concerns with your dentist ahead of time. They may be able to use smaller sensors or recommend relaxation techniques to make the process more comfortable.
2. During the X-Ray: What to Expect
- Positioning:
- You will be seated in a dental chair, and your dentist or dental assistant will position you for the X-ray. They may ask you to bite down on a small sensor or film holder, which will be placed inside your mouth. The sensor may feel slightly uncomfortable, but it should only be in place for a few moments.
- Lead Apron and Thyroid Collar:
- To protect your body from unnecessary radiation, you will likely be draped with a lead apron and, in some cases, a thyroid collar. These shields are designed to block radiation from reaching other parts of your body.
- Brief and Painless Process:
- The actual X-ray exposure takes just a few seconds. You’ll need to remain still while the X-ray is being taken to ensure a clear image. The entire process is painless, though the sensor or film holder may cause mild discomfort.
- X-ray Machine Setup:
- Intraoral X-rays: For periapical views, an intraoral X-ray machine is used. The X-ray device is positioned inside the mouth to capture images of individual teeth.
- Bitewing X-rays: These views, focusing on the upper and lower back teeth, involve the patient biting down on a special X-ray film holder.
- Panoramic or CBCT X-rays: These provide a broader view and are captured with the patient’s head positioned in a specific alignment within the X-ray machine.
- X-ray Capture:
- Intraoral X-rays: The X-ray machine is activated for a brief moment, and the image receptor or film captures the X-rays that pass through the teeth.
- Bitewing X-rays: The patient holds the film holder in place, and X-rays are directed through the teeth onto the film.
- Panoramic or CBCT X-rays: The machine rotates around the head, capturing images from various angles to create a comprehensive view.
- Image Processing:
- Traditional X-rays: The captured X-ray images are processed and developed using traditional film-based methods.
- Digital X-rays: In modern practices, digital sensors or phosphor plates are used, and the images are processed digitally for immediate viewing.
- Multiple Images:
- Depending on the complexity of your case, your dentist may need to take multiple X-rays from different angles. This ensures a comprehensive view of the tooth and surrounding structures.
- Review and Analysis:
- Dentist’s Evaluation: The dentist reviews the X-ray images to assess tooth structures, root canals, surrounding bone, and any potential issues.
- Discussion with Patient: The dentist discusses the findings with the patient, explaining any identified concerns and the recommended treatment plan.
3. After the X-Ray: Follow-up Care
- No Special Care Needed:
- Typically, no special care is needed after a root canal X-ray. You can return to your normal activities immediately after the procedure.
- Discuss Results with Your Dentist:
- Your dentist will review the X-ray images with you, explaining any findings and discussing the next steps in your treatment plan. This might include a root canal procedure, further diagnostic tests, or other dental treatments.
- Address Any Discomfort:
- If the X-ray process caused any mild discomfort or soreness in your mouth, it should subside quickly. If you experience any lingering discomfort, discuss it with your dentist.
- Regular Dental Check-Ups:
- Regular dental visits and routine X-rays (as recommended by your dentist) help maintain oral health and detect any issues early. This is particularly important if you have had root canal therapy, as follow-up X-rays may be needed to monitor the healing process.
Preparing for a root canal X-ray is straightforward, and understanding what to expect can help make the experience stress-free. By following these practical tips, you can ensure a smooth process, receive accurate results, and continue with any necessary dental care promptly. Your dentist is there to guide you through each step, so don’t hesitate to ask questions or express any concerns you might have.
Interpreting Root Canal X-rays

Root canal X-rays play a pivotal role in aiding dentists to diagnose and plan treatments for dental issues. Proper interpretation of these X-rays is essential for understanding the condition of the tooth and surrounding structures. Here’s a guide to help in interpreting root canal X-ray images:
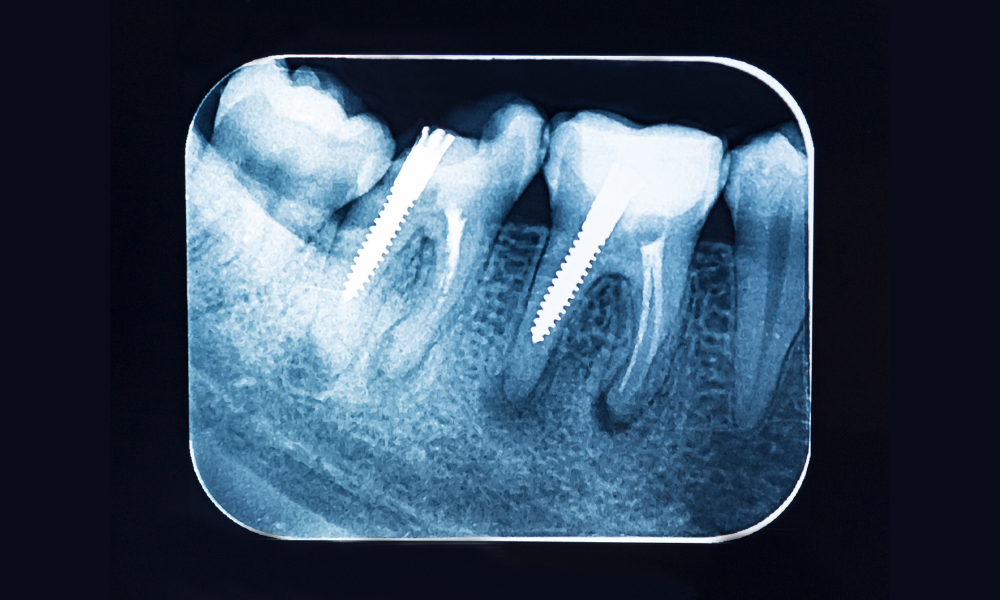
- Tooth Structure Assessment: The X-ray provides a clear view of the crown (visible part) and the root (hidden below the gumline) of the tooth. Dentists assess these structures for signs of decay, fractures, or abnormalities.
- Root Canal Anatomy: Dentists examine the root canal space for any signs of infection, inflammation, or abnormalities. This includes identifying the number of canals within a tooth.
- Bone Health: The periapical area, representing the region around the tooth’s tip, is assessed for bone density and any changes. Bone loss or irregularities may indicate infection or periodontal issues.
- Periodontal Ligament Condition: The periodontal ligament, connecting the tooth to the jawbone, is visible on X-rays. Changes in this space may indicate issues such as tooth mobility or gum disease.
- Apical Health: Dentists identify the apical foramen, the opening at the tip of the tooth’s root where nerves and blood vessels enter. Changes in this area may signal infection or complications.
- Previous Dental Work: X-rays reveal existing dental work, such as fillings or crowns. Dentists assess their condition and integrity, looking for signs of wear, decay, or the need for replacement.
- Abnormalities or Anomalies: Unusual root canal configurations or extra canals may be identified through X-rays. Dentists evaluate these anomalies for potential treatment considerations.
- Contralateral Teeth: Comparing X-rays of the affected tooth with those of contralateral (opposite) teeth helps dentists identify discrepancies and abnormalities more effectively.
- Treatment Planning: X-rays guide dentists in planning and performing root canal therapy. The images help determine the length and shape of the root canals, ensuring thorough cleaning and sealing.
- Patient Consultation: Dentists use X-rays as visual aids during patient consultations, explaining identified issues and proposed treatment plans comprehensively.
Effective interpretation of root canal X-rays requires a trained eye and a comprehensive understanding of dental anatomy. Dentists leverage these insights to deliver precise diagnoses and develop tailored treatment strategies, ensuring optimal oral health for their patients.
Root Canal X-rays and Treatment Success
Root canal X-rays play a crucial role in the success of root canal treatment, a procedure aimed at saving a severely damaged or infected tooth. These X-rays, also known as endodontic X-rays, provide valuable insights for dentists to ensure the effectiveness of the treatment. Here’s how root canal X-rays contribute to treatment success:
- Identifying Issues: Root canal X-rays help dentists accurately diagnose the extent of infection, the number of affected canals, and any associated complications. This precision guides the development of a targeted treatment plan.
- Detailed Treatment Planning: X-rays reveal the internal structure of the tooth, including the root canal anatomy. This information is vital for dentists to plan the treatment, ensuring all canals are thoroughly cleaned, disinfected, and sealed.
- Locating Infections: X-rays provide a visual representation of infection or abscesses in and around the tooth’s root. Dentists use this information to target and eliminate the source of infection during the root canal procedure.
- Monitoring Treatment Progress: Throughout the treatment process, dentists may take follow-up X-rays to assess changes in the tooth and surrounding structures. This allows them to ensure that the infection is being effectively eliminated.
- Ensuring Complete Cleaning: X-rays confirm the thorough cleaning of the root canals. This step is crucial to remove all traces of infection and prevent its recurrence, promoting the long-term success of the treatment.
- Sealing the Canals: X-rays assist in evaluating the quality of the canal sealing. A proper seal is essential to prevent reinfection and maintain the structural integrity of the treated tooth.
- Identifying Complications: X-rays help dentists identify any complications or challenges during or after the root canal procedure. Timely detection allows for prompt intervention, preventing potential treatment failures.
- Comparing Pre and Post X-rays: Comparing X-rays taken before and after the root canal treatment enables dentists to assess the success of the procedure. Positive changes, such as reduced infection and improved bone density, indicate treatment success.
- Patient Consultation: Dentists use X-rays as visual aids during consultations with patients. Showing the improvements achieved through root canal treatment helps patients understand the success of the procedure and promotes oral health awareness.
Root canal X-rays are an integral part of the endodontic process, contributing to the overall success and longevity of the treatment. Through precise diagnosis, detailed treatment planning, and continuous evaluation, dentists leverage X-rays to ensure optimal outcomes and the preservation of natural teeth.
Challenges and Limitations of Root Canal X-rays
While root canal X-rays are invaluable in diagnosing and treating dental issues, they come with certain challenges and limitations that dentists need to navigate. Understanding these aspects is crucial for both dental professionals and patients. Here are some challenges and limitations associated with root canal X-rays:
- Two-Dimensional Imaging: X-rays provide a two-dimensional view, making it challenging to visualize complex three-dimensional structures accurately. This limitation may affect the assessment of canal anatomy and potential variations.
- Inability to Capture Pain Perception: X-rays cannot capture pain perception. Patients may experience pain or discomfort that is not visible on the X-ray images, requiring additional communication and evaluation methods.
- Concerns for Some Patients: Despite advancements in reducing radiation doses, some patients may still have concerns about exposure. Dentists must address these concerns and use X-rays judiciously, following established safety protocols.
- Missed Small Apical Lesions: Small apical lesions, especially in the early stages, may be challenging to detect on X-rays. This can lead to a delay in diagnosis and treatment, impacting the overall success of root canal therapy.
- Interpretation Variability: Interpreting X-ray images involves a degree of subjectivity. Different practitioners may have variations in interpretation, potentially leading to differences in treatment approaches.
- Overlapping Structures: Overlapping anatomical structures, such as adjacent teeth or bone, can obstruct the view of specific areas. This may hinder the accurate assessment of the root canal system.
- Limited Soft Tissue Information: X-rays primarily focus on hard tissues like teeth and bone, providing limited information about soft tissues. Soft tissue conditions, such as inflammation or lesions, may not be fully captured.
- Variability in Patient Anatomy: Patient anatomy varies, and some individuals may have anatomical complexities that make it challenging to obtain clear X-ray images. Adapting to these variations is essential for accurate diagnosis.
- Risk of Overlooking Early Lesions: Small or early lesions may not be visible on X-rays, leading to potential oversight. Dentists must consider clinical symptoms and other diagnostic tools for a comprehensive assessment.
- Dependency on Operator Skill: The quality and diagnostic value of root canal X-rays are influenced by the operator’s skill in positioning and capturing images. Inexperienced operators may encounter challenges in obtaining optimal X-rays.
Despite these challenges, root canal X-rays remain a crucial diagnostic tool in endodontics. Dental professionals must recognize these limitations, use X-rays judiciously, and complement their findings with clinical evaluation and patient symptoms for a comprehensive understanding of the root canal condition. Open communication between dentists and patients about the benefits and limitations of X-rays is essential for informed decision-making in dental care.
Root Canal X-rays in Pediatric Dentistry
Pediatric dentistry involves unique considerations, and the use of root canal X-rays in children requires a tailored approach. Here are key aspects to understand regarding the application of root canal X-rays in pediatric dentistry:
- Indications for Root Canal X-rays: Root canal X-rays in pediatric patients are selectively employed based on clinical indications. These include cases of dental trauma, severe tooth decay, or suspected pulpal involvement.
- Radiation Safety Measures: Due to the sensitivity of developing tissues, minimizing radiation exposure is paramount. Dentists follow strict protocols, including the use of lead aprons and thyroid collars, to ensure the safety of young patients during X-ray procedures.
- Techniques for Cooperation: Pediatric dentists employ child-friendly communication and behavior management techniques to ensure cooperation during X-ray procedures. This may involve explaining the process in a simple manner and using comforting language.
- Diagnostic Value in Primary Teeth: Root canal X-rays play a crucial role in assessing the condition of the pulp in primary (baby) teeth. They aid in diagnosing issues such as pulpitis or abscesses, guiding appropriate treatment decisions.
- Follow-up Assessments: Root canal X-rays are utilized for follow-up assessments after pediatric endodontic treatments. They help evaluate the success of the treatment and ensure the health of the treated tooth.
- Collaboration with Parents: Dentists collaborate with parents to explain the necessity and benefits of root canal X-rays. Open communication ensures that parents are well-informed about the procedure and can make informed decisions regarding their child’s dental care.
- Adapting to Child’s Anatomy: Pediatric dentists are well-versed in the anatomical variations seen in children. Adapting X-ray techniques to accommodate smaller oral structures ensures optimal imaging quality.
- Complementary Approaches: In some cases, where X-rays pose challenges, alternative diagnostic tools such as clinical examination, pulp testing, and intraoral cameras may be employed to gather comprehensive information.
- Patient and Parent Education: Pediatric dentists take the opportunity to educate both young patients and their parents about the importance of maintaining oral health. This includes discussions on preventive measures and the role of root canal X-rays in ensuring dental wellness.
Root canal X-rays in pediatric dentistry align with the principles of minimally invasive and patient-centered care. By customizing approaches to suit the unique needs of children and prioritizing safety, dental professionals can effectively utilize root canal X-rays as a valuable tool in managing oral health challenges in the pediatric population.
Potential Risks and Complications Associated with Root Canal X-Rays and How to Minimize Them
While root canal X-rays are essential diagnostic tools in dentistry, like all medical procedures, they come with some potential risks and complications. Understanding these risks, however, can help mitigate them and ensure that the benefits of X-ray imaging far outweigh any negatives.
1. Radiation Exposure
Risk:
One of the most well-known risks associated with X-rays, including those used in root canal procedures, is radiation exposure. Although dental X-rays emit relatively low levels of radiation compared to other medical imaging techniques, repeated exposure over time can still pose a cumulative risk, potentially increasing the chance of developing radiation-related health issues.
Minimization Strategies:
- Use of Lead Aprons and Thyroid Collars: To protect patients from unnecessary exposure, dental professionals routinely use lead aprons and thyroid collars. These barriers shield the body’s most sensitive areas, such as the thyroid gland and reproductive organs, from radiation.
- Digital X-Rays: Transitioning from traditional film X-rays to digital X-rays can significantly reduce radiation exposure. Digital X-rays require up to 90% less radiation and also offer enhanced image quality, which aids in more accurate diagnosis.
- As Low As Reasonably Achievable (ALARA) Principle: This principle emphasizes minimizing radiation exposure by using the lowest possible radiation dose that still provides clear diagnostic images. Dentists follow this principle by carefully selecting the type and frequency of X-rays based on the patient’s specific needs.
2. Potential for Overuse
Risk:
The convenience and diagnostic power of X-rays can sometimes lead to their overuse. While X-rays are critical for diagnosing certain dental conditions, unnecessary or frequent X-rays may expose patients to avoidable radiation, especially when alternative diagnostic methods could suffice.
Minimization Strategies:
- Individualized Treatment Plans: Dentists should tailor X-ray usage to each patient’s individual needs, avoiding routine or unnecessary X-rays unless clinically justified. This approach reduces exposure while still ensuring that the necessary diagnostic information is obtained.
- Regular Review of Protocols: Dental practices should periodically review their X-ray protocols and guidelines to ensure they align with the latest evidence-based recommendations. This ensures that X-rays are only used when absolutely necessary.
3. Potential Discomfort During X-Ray Procedures
Risk:
Some patients may experience discomfort during the placement of X-ray sensors or films in their mouths, particularly with periapical or bitewing X-rays. This discomfort can be more pronounced in patients with a strong gag reflex, small mouths, or oral sensitivities.
Minimization Strategies:
- Use of Smaller Sensors or Film Holders: For patients who experience discomfort, dentists can use smaller or more flexible sensors that are easier to position and less likely to cause discomfort.
- Patient Positioning and Relaxation Techniques: Proper patient positioning and guiding patients through relaxation techniques can help minimize discomfort. For instance, instructing patients to breathe through their noses or using distraction techniques can make the process smoother.
- Explaining the Procedure: Ensuring that patients understand what to expect during the X-ray process can reduce anxiety and discomfort. Clear communication about the purpose and process of the X-ray can help patients feel more comfortable.
4. Allergic Reactions to X-Ray Materials
Risk:
In rare cases, patients may have allergic reactions to materials used during the X-ray process, such as latex in gloves or materials used in X-ray sensors.
Minimization Strategies:
- Use of Hypoallergenic Materials: Dental practices can mitigate this risk by using hypoallergenic gloves and other materials. Communicating with patients about any known allergies before the procedure allows dentists to take appropriate precautions.
- Monitoring for Reactions: Dental professionals should monitor patients for any signs of an allergic reaction during and after the X-ray procedure, ready to intervene if necessary.
5. Misinterpretation of X-Ray Results
Risk:
While not a direct physical risk, the potential for misinterpretation of X-ray results can lead to incorrect diagnoses or inappropriate treatment plans. This can result in unnecessary procedures, delays in proper treatment, or failure to address the underlying issue.
Minimization Strategies:
- Advanced Training for Dentists: Ensuring that dental professionals have advanced training in reading and interpreting X-rays is crucial for accurate diagnosis and treatment planning.
- Use of Advanced Imaging Technology: Incorporating more advanced imaging techniques, such as CBCT scans when necessary, can provide more detailed and accurate views of the tooth and surrounding structures, reducing the likelihood of misinterpretation.
While root canal X-rays are generally safe and indispensable in diagnosing and treating dental issues, it’s important to be aware of the potential risks and complications associated with their use. By implementing strategies to minimize radiation exposure, ensure patient comfort, and improve the accuracy of diagnosis, dental professionals can maximize the benefits of X-rays while minimizing any associated risks. Through careful planning, education, and the use of modern technology, both patients and dentists can feel confident in the safe and effective use of root canal X-rays.
Patient Education and Informed Consent
In the realm of healthcare, particularly dentistry, patient education and informed consent are foundational components that empower individuals to actively participate in their own care. Here’s a detailed exploration of the significance, elements, and ethical considerations associated with patient education and informed consent:
1. Significance of Patient Education:
- Empowering Decision-Making: Patient education is a process that equips individuals with information about their health conditions, treatment options, and potential outcomes. This knowledge empowers patients to make informed decisions aligned with their preferences and values.
2. Elements of Effective Patient Education:
- Clear Communication: Effective patient education involves clear and jargon-free communication. Healthcare providers should convey information in a manner that is easily understandable, considering the patient’s literacy level and cultural background.
3. Role of Informed Consent:
- Legal and Ethical Foundation: Informed consent is a legal and ethical requirement in healthcare. It involves obtaining permission from a patient after providing comprehensive information about the proposed treatment, potential risks, alternatives, and anticipated outcomes.
4. Components of Informed Consent:
- Nature of the Procedure: The healthcare provider explains the nature and purpose of the procedure or treatment.
- Risks and Benefits: Patients are informed about the potential risks, benefits, and alternative options available.
- Expected Outcomes: The likely outcomes and potential complications are discussed to manage patient expectations.
- Voluntariness: Informed consent must be given voluntarily, without coercion or undue influence.
5. Shared Decision-Making:
- Collaborative Approach: Patient education facilitates shared decision-making, where healthcare providers and patients collaboratively discuss and decide on the most suitable treatment plan. This approach respects the autonomy and preferences of the patient.
6. Communication Challenges and Solutions:
- Language and Literacy: Language barriers and low health literacy can impede effective communication. Healthcare providers should employ interpreters, visual aids, and written materials in plain language to enhance understanding.
7. Cultural Competence:
- Respecting Diversity: Cultural competence is crucial in patient education. Understanding and respecting diverse cultural beliefs and practices ensures that information is conveyed in a culturally sensitive manner.
8. Technological Tools in Patient Education:
- Digital Resources: With advancements in technology, digital tools such as videos, interactive apps, and online resources play a role in patient education. These tools can enhance comprehension and engagement.
9. Evolving Legal Landscape:
- Documentation and Accountability: In an evolving legal landscape, healthcare providers must document the informed consent process thoroughly. This documentation serves as evidence of the patient’s understanding and agreement to the proposed treatment.
10. Continuous Communication:
- Ongoing Dialogue: Patient education is not a one-time event but an ongoing process. Regular and open communication between healthcare providers and patients ensures that any evolving aspects of the treatment plan are discussed and understood.
Patient education and informed consent are integral to ethical and patient-centered healthcare. By prioritizing clear communication, respecting cultural diversity, and embracing technological advancements, healthcare providers can foster a collaborative and informed healthcare journey with their patients.
Final Words
Root canal X-rays are invaluable tools in the realm of endodontics, providing essential insights for diagnosis, treatment planning, and postoperative evaluation. Their judicious use, coupled with advancements in digital technology, contributes to the success of root canal procedures and the overall oral health of patients. Regular communication between dentists and patients fosters understanding, trust, and collaborative decision-making in the journey toward optimal dental care.
References
1. Textbooks
- “Pathways of the Pulp” by Stephen Cohen and Kenneth M. Hargreaves: This textbook is a comprehensive resource on endodontics, covering diagnostic techniques, including X-rays, and their role in root canal therapy.
- “Endodontics: Principles and Practice” by Mahmoud Torabinejad and Richard E. Walton: This book provides detailed information on endodontic procedures, including the use of radiography in root canal treatments.
Online Resources
- American Dental Association (ADA) Website: The ADA’s website offers resources and information on dental practices, including the use of X-rays in various dental treatments.