Lateral finger X-ray imaging is a valuable diagnostic tool for assessing various conditions affecting the fingers, from fractures to joint abnormalities. This guide is tailored for radiographers, providing insights into the intricacies of obtaining optimal lateral finger X-ray images for accurate and comprehensive diagnostics.
Table of Contents
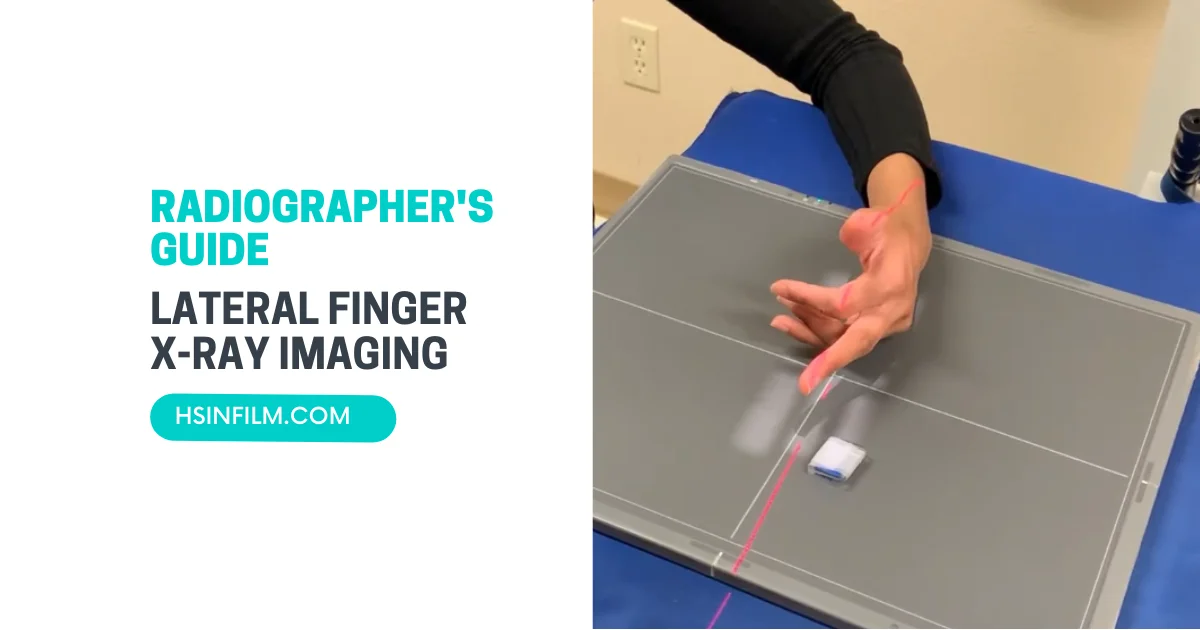
Patient Positioning for Lateral Finger X-ray
Accurate patient positioning is crucial to obtaining clear and diagnostically valuable lateral finger X-rays. Proper positioning ensures optimal visualization of the finger anatomy, aiding healthcare professionals in identifying fractures, dislocations, or other abnormalities. Here is a step-by-step guide for the patient positioning in a lateral finger X-ray:
1. Preparation
- Explanation and Communication: Explain the procedure to the patient, including the importance of staying still during the X-ray to avoid blurring.
- Patient Attire: Ensure the patient removes any jewelry, watches, or metal objects from the hand or finger being imaged to prevent interference with the X-ray.
2. Positioning
- Patient Standing or Seated: The patient can either stand beside the X-ray machine or be seated on a stool, depending on their comfort and the facility’s equipment.
- Side of Interest Facing the X-ray Machine: Instruct the patient to position the side of the finger of interest facing the X-ray machine. If it’s the right finger, the right side should face the machine, and vice versa.
- Elbow Flexion: Ask the patient to flex their elbow at approximately 90 degrees. This helps align the finger properly and minimizes superimposition of other structures.
- Hand Placement: Place the palm of the hand flat on the imaging receptor or the X-ray table, with the fingers extended and close together. Ensure the finger of interest is centered over the imaging area.
- Finger Extension: Instruct the patient to extend the finger of interest fully. This helps in obtaining a clear and unobstructed view of the entire finger, including the joints.
- Collimate: Adjust the collimation field to focus only on the finger being imaged, limiting unnecessary radiation exposure to surrounding areas.
3. X-ray Beam Direction
Ensure that the X-ray beam is directed perpendicularly to the imaging receptor and the finger. This helps minimize distortion and ensures accurate representation of the anatomy.
4. Lead Shielding
Place lead shielding on areas not being imaged to reduce radiation exposure to adjacent tissues. This includes the hand, wrist, and forearm of the opposite side.
5. Image Capture
- Patient Cooperation: Instruct the patient to remain as still as possible during image capture to prevent motion artifacts.
- X-ray Exposure: Capture the X-ray image with the specified exposure settings, ensuring proper penetration and clarity.
6. Labeling and Documentation
Properly label the X-ray with patient information, date, and finger side (right or left). Document any relevant clinical information or concerns.
By adhering to these positioning guidelines, healthcare professionals can obtain high-quality lateral finger X-rays, aiding in accurate diagnoses and appropriate treatment planning.
Also read: Guide to Efficient X-ray Control Panel
Collimation and Focus for Lateral Finger X-ray
Collimation and focus are critical aspects of obtaining high-quality lateral finger X-rays. These factors ensure precise imaging, reduced radiation exposure to non-target areas, and improved diagnostic accuracy. Here’s a guide on collimation and focus considerations for lateral finger X-rays:
1. Collimation
- Definition: Collimation refers to the process of restricting the X-ray beam to the area of interest, minimizing unnecessary exposure to adjacent tissues.
- Purpose: The primary goal of collimation is to enhance image quality by reducing scatter radiation, improving contrast, and focusing the X-ray beam specifically on the finger being imaged.
- Adjustable Collimators: Use X-ray machines equipped with adjustable collimators. This allows healthcare professionals to customize the size and shape of the X-ray beam according to the dimensions of the finger.
- Collimation Field: Set the collimation field to encompass only the finger of interest, excluding surrounding structures. This ensures a clear and detailed image while minimizing radiation exposure to non-relevant areas.
- Collimator Blades: Align the collimator blades to the longitudinal and transverse axes of the finger. This precision helps maintain clarity and prevents unnecessary radiation dispersion.
2. Focus
- Focal Spot Size: The focal spot size represents the area on the anode where X-rays are generated. Opt for a smaller focal spot size for improved spatial resolution and sharper images.
- Source-to-Image Distance (SID): Maintain an appropriate source-to-image distance (SID), which is the distance between the X-ray tube and the image receptor. Adequate SID helps maintain image clarity and minimizes distortion.
- Positioning the X-ray Tube: Align the X-ray tube perpendicular to the imaging receptor and the finger. This ensures accurate representation of the finger anatomy and minimizes geometric distortion.
- Focal Spot-to-Image Receptor Distance: Keep the focal spot-to-image receptor distance consistent to maintain optimal image quality. Deviations from the recommended distance can affect resolution and clarity.
- Centering the X-ray Beam: Center the X-ray beam precisely over the finger of interest. Proper centering ensures uniform exposure and avoids unnecessary radiation to adjacent structures.
- Adjusting Parameters: Fine-tune exposure parameters, such as mAs and kVp, based on the specific requirements of the lateral finger X-ray. Consult with the facility’s protocols and imaging guidelines.
By adhering to meticulous collimation and focus practices, healthcare professionals can optimize lateral finger X-rays, obtaining clear and diagnostically valuable images while prioritizing patient safety through minimized radiation exposure.
Radiation Safety Measures for Lateral Finger X-ray
Ensuring radiation safety is paramount during medical imaging procedures, including lateral finger X-rays. Implementing effective safety measures helps minimize radiation exposure to both healthcare professionals and patients. Here’s a comprehensive guide on radiation safety measures for lateral finger X-rays:
- Use of Lead Aprons and Thyroid Shields: Healthcare professionals should wear lead aprons to shield their bodies from scattered radiation. Additionally, thyroid shields protect the thyroid gland, a sensitive organ, from unnecessary exposure.
- Protective Gonadal Shielding: When imaging reproductive organs is not necessary, protective gonadal shielding should be employed. This is particularly important for patients of reproductive age to reduce radiation exposure to the gonads.
- Collimation Optimization: Ensure proper collimation to restrict the X-ray beam to the area of interest. This minimizes unnecessary exposure to surrounding tissues and organs.
- Patient Positioning: Precise patient positioning is crucial. Ensure accurate alignment of the finger with the X-ray beam to avoid repeat exposures, which could increase radiation dose.
- Lead Gloves and Radiation Attenuating Gloves: Healthcare professionals handling X-ray equipment should wear lead gloves or radiation attenuating gloves to protect their hands from direct exposure.
- Minimization of Exposure Time: Keep exposure time as short as reasonably achievable (ALARA). Minimizing the duration of X-ray exposure reduces the overall radiation dose.
- Source-to-Skin Distance (SSD): Maintain an appropriate source-to-skin distance (SSD) to optimize image quality while limiting radiation dose. Adequate SSD ensures consistent and accurate imaging.
- Proper X-ray Tube Positioning: Position the X-ray tube accurately to maintain the recommended angles and distances. This prevents unnecessary radiation dispersion and ensures focused imaging.
- Use of High-Speed Film or Digital Detectors: Utilize high-speed film or digital detectors, which require shorter exposure times. This reduces the duration of radiation exposure without compromising image quality.
- Quality Assurance Programs: Implement quality assurance programs to regularly assess and maintain the performance of X-ray equipment. This ensures that equipment operates optimally and consistently delivers safe and high-quality images.
By adhering to these radiation safety measures, healthcare facilities can perform lateral finger X-rays with a focus on patient and staff safety, achieving diagnostic goals while minimizing radiation risks. Regular training, ongoing quality assurance, and the use of advanced technologies contribute to maintaining a safe and effective imaging environment.
Image Receptor Placement for Lateral Finger X-ray
Accurate image receptor placement is essential for obtaining clear and diagnostically valuable lateral finger X-ray images. Proper positioning ensures optimal visualization of the finger anatomy, aiding healthcare professionals in making accurate assessments. Here is a step-by-step guide on image receptor placement for lateral finger X-ray:
- Patient Positioning: Instruct the patient to stand or sit comfortably, depending on the facility’s equipment and protocols. Ensure that the patient is relaxed and can maintain the required position during the X-ray procedure.
- Identify the Finger of Interest: Confirm which finger requires imaging. Ensure that the correct finger is identified, and communicate with the patient to avoid any misunderstandings.
- Remove Jewelry and Accessories: Ask the patient to remove any jewelry, watches, or accessories from the finger undergoing X-ray. Metallic objects can interfere with the imaging process and obscure details.
- Collimate to the Area of Interest: Adjust the X-ray collimator to focus the beam specifically on the finger of interest. Collimation minimizes unnecessary radiation exposure to surrounding tissues and ensures a well-defined image.
- Secure Image Receptor: Place the image receptor (film or digital detector) against the side of the finger opposite the X-ray tube. Ensure that the receptor is securely positioned and won’t move during exposure.
- Finger Alignment: Instruct the patient to extend the finger fully. Align the finger parallel to the image receptor for a lateral view. The finger should be straight, with the joint spaces open and visible.
- Maintain Consistent Technique: Follow consistent exposure techniques to ensure uniform image quality across different patients. This includes consistent X-ray tube settings and exposure times.
- Include Proximal and Distal Joints: Ensure that the X-ray beam encompasses both the proximal and distal interphalangeal joints. This comprehensive view aids in assessing the entire finger anatomy for potential abnormalities or injuries.
- Source-to-Image Distance (SID): Maintain the recommended source-to-image distance (SID) to achieve optimal magnification and clarity in the X-ray image. SID is the distance between the X-ray tube and the image receptor.
- Beam Centering: Center the X-ray beam over the finger of interest. Proper beam centering ensures that the anatomy is well-visualized without unnecessary radiation exposure to adjacent structures.
By following these steps, healthcare professionals can ensure precise image receptor placement for lateral finger X-rays, obtaining high-quality images that contribute to accurate diagnoses and treatment planning. Consistency in positioning and attention to detail are key factors in achieving optimal results.
Hand and Finger Immobilization for Lateral Finger X-ray

Effective hand and finger immobilization is crucial during a lateral finger X-ray to achieve clear and diagnostic images while minimizing motion artifacts. Proper immobilization ensures that the finger remains still throughout the imaging process, resulting in high-quality radiographs. Here are the steps for hand and finger immobilization during a lateral finger X-ray:
- Explain the Procedure: Communicate clearly with the patient, explaining the need for immobilization to obtain accurate X-ray images. Address any concerns or questions the patient may have.
- Position the Patient: Instruct the patient to stand or sit comfortably, depending on the facility’s protocols and the patient’s ability to maintain the required position.
- Secure the Hand: Gently secure the patient’s hand using a positioning aid or foam block. The foam block should provide support and stability to keep the hand in the desired lateral position.
- Align the Finger: Align the finger of interest parallel to the image receptor, ensuring that the joint spaces are open and visible. The finger should be straight for a lateral view.
- Use Immobilization Devices: Depending on the facility’s equipment, use immobilization devices such as sandbags, straps, or specialized finger holders to prevent unintentional movement. These devices help maintain consistent positioning.
- Secure the Finger: Secure the finger firmly in place using the chosen immobilization device. Straps can be used across the hand or around the finger to prevent any lateral or rotational movement.
- Remove Jewelry: Ensure that the patient has removed any jewelry, watches, or accessories from the finger undergoing X-ray. Metallic objects can interfere with the imaging process and cause artifacts.
- Check for Stability: Before proceeding with the X-ray, double-check that the hand and finger are stable and properly immobilized. Any unintended movement during exposure can compromise image quality.
By following these steps, healthcare professionals can achieve effective hand and finger immobilization for lateral finger X-rays. This approach ensures consistent and motion-free images, facilitating accurate diagnoses and contributing to the overall safety and well-being of the patient.
Marker Placement for Identification in Lateral Finger X-ray
The proper placement of markers is essential in medical imaging to provide accurate identification and orientation of anatomical structures on X-ray images. In a lateral finger X-ray, markers are used to indicate the side of the body, specific digits, and the orientation of the image. Here are the key steps for marker placement during a lateral finger X-ray:
- Side Marking: Begin by identifying the side of the finger being imaged. Typically, a small, lead-free marker with the letter “L” or “R” is used to indicate the left or right side. Place this marker on the side of the finger to provide clear laterality information.
- Digit Numbering: To distinguish between different fingers, a numeric marker is often used. Place a lead-free marker with the appropriate digit number (e.g., “2” for the index finger) on the region of interest. This helps in identifying the specific finger being examined.
- Orientation Marker: Include an orientation marker to indicate the direction of the X-ray beam. This marker often consists of an arrow or a specific design. Place it adjacent to the finger being imaged, pointing in the direction of the X-ray source. This aids radiologists in understanding the orientation of structures in the final image.
- Consistent Placement: Ensure consistent and standardized marker placement for all lateral finger X-rays within the facility. This practice enhances the efficiency of image interpretation and reduces the likelihood of errors.
- Clear Visibility: Position the markers close to the region of interest, making them clearly visible on the X-ray images. Avoid placing markers over bony anatomy or areas that may obscure important details.
- Artifact-Free Placement: Be mindful of the placement to avoid introducing artifacts into the X-ray image. Artifacts can affect the clarity of the image and hinder accurate diagnosis.
- Document Marker Placement: Include documentation of marker placement in the patient’s medical records. This information is valuable for future reference, comparisons, and follow-up examinations.
By adhering to these guidelines, healthcare professionals can ensure that markers are appropriately placed during lateral finger X-rays. Consistent and accurate marker placement contributes to the overall quality of radiographic images and aids in precise anatomical identification during interpretation.
Evaluation of Soft Tissues in Lateral Finger X-ray
Proper interpretation of soft tissue details is crucial for a comprehensive understanding of the patient’s condition. Here are key aspects to consider when evaluating soft tissues in a lateral finger X-ray:
- Skin and Subcutaneous Tissues: The skin and subcutaneous tissues appear as a continuous, uniform layer surrounding the finger. Assess for any abnormalities, such as swelling, masses, or skin lesions.
- Soft Tissue Swelling: Soft tissue swelling may indicate inflammation or trauma. Evaluate the thickness and symmetry of soft tissues, comparing them to the contralateral side for reference.
- Joint Spaces: Examine the joint spaces between the bones of the finger. Normal joint spaces should appear as uniform, well-defined gaps. Irregularities or widening may suggest joint effusion or arthritis.
- Tendons and Ligaments: Tendons and ligaments are not directly visible on X-rays but may indirectly indicate abnormalities through their impact on adjacent bone structures. Evaluate for any signs of avulsion fractures, which may result from forceful tendon or ligament contractions.
- Soft Tissue Calcifications: Calcifications within the soft tissues may be visible on X-rays. These can result from conditions such as calcific tendinitis or soft tissue calcifications associated with systemic disorders.
- Foreign Bodies: Soft tissue X-rays can reveal the presence of foreign bodies, such as glass or metal fragments. Assess for any radiopaque objects that may be embedded in the soft tissues.
- Joint Effusion: Joint effusion, characterized by the accumulation of fluid within the joint space, may manifest as soft tissue widening adjacent to the affected joint. Evaluate for signs of joint effusion, which may be indicative of an underlying pathology.
- Soft Tissue Masses: Soft tissue masses, tumors, or cysts may be visible on X-rays. These can present as areas of soft tissue density with well-defined or irregular borders. Further imaging modalities, such as ultrasound or MRI, may be necessary for a more detailed assessment.
- Symmetry and Alignment: Compare the soft tissues on the lateral finger X-ray with the contralateral side for symmetry. Asymmetry may indicate localized abnormalities.
Radiologists and healthcare professionals should approach the evaluation of soft tissues in lateral finger X-rays with a systematic and detailed assessment. Combining the analysis of bony and soft tissue structures enhances the diagnostic accuracy and ensures a comprehensive evaluation of the finger’s health.
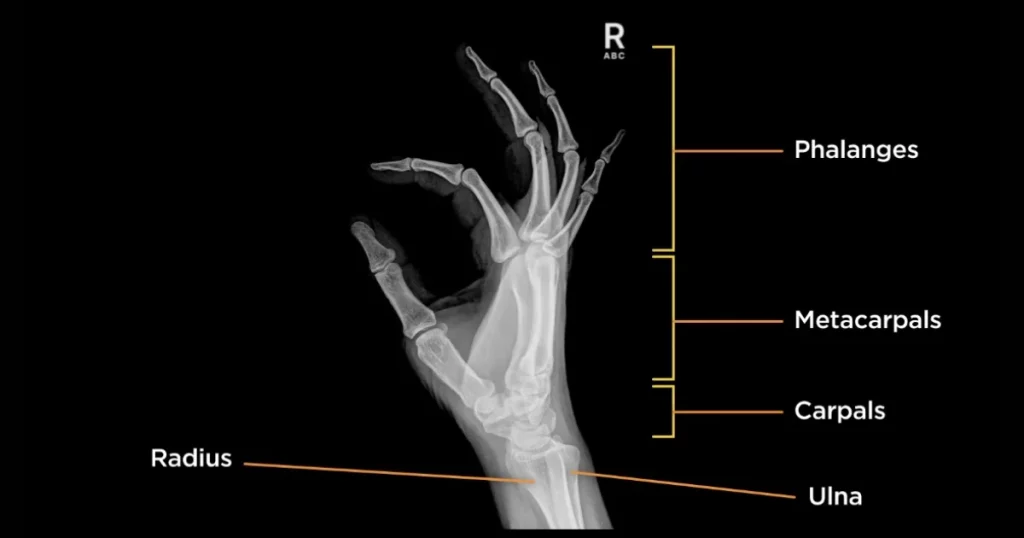
Evaluating Joint Spaces and Bony Landmarks in Lateral Finger X-ray
In a lateral finger X-ray, a detailed assessment of joint spaces and bony landmarks is crucial for identifying abnormalities and understanding the overall health of the finger. Here are key considerations when evaluating joint spaces and bony landmarks in a lateral finger X-ray:
- Metacarpophalangeal (MCP) Joints: The MCP joints, located between the metacarpal bones and the proximal phalanges, should exhibit uniform joint spaces. Assess for any signs of joint space narrowing, which may indicate arthritis, or joint space widening, suggestive of joint effusion.
- Proximal and Distal Interphalangeal (PIP and DIP) Joints: Similar to the MCP joints, the PIP and DIP joints should display clear and symmetrical joint spaces. Irregularities in joint spacing, such as osteophyte formation or erosion, may be indicative of degenerative joint diseases.
- Articular Surfaces: Examine the articular surfaces of the phalanges and metacarpals for smooth contours. Irregularities or deformities in the bone surfaces may suggest fractures, dislocations, or underlying joint pathology.
- Carpometacarpal (CMC) Joint of the Thumb: Evaluate the CMC joint of the thumb for any signs of arthritis, subluxations, or osteophyte formation. Changes in this joint can impact thumb function and overall hand mobility.
- Soft Tissue Alignments: Assess soft tissue alignments, such as the alignment of tendons and ligaments, in relation to the joint spaces. Disruptions in soft tissue alignments may indicate injuries or abnormalities affecting the adjacent joints.
- Cortical Bone Integrity: Ensure the cortical bone of the phalanges and metacarpals appears intact without evidence of fractures. Fractures may present as discontinuities or irregularities in the bone cortex.
- Base and Shaft of Phalanges: Examine the bases and shafts of the phalanges for any signs of bone resorption, sclerosis, or deformities. Abnormalities in these areas may be indicative of various pathological conditions.
- Cortical Thickness: Assess the thickness of the cortical bone. Variations in cortical thickness may suggest conditions such as osteopenia or osteoporosis.
- Proximal Metacarpal Articulations: Evaluate the articulations between the proximal metacarpals for any signs of degeneration, such as joint space narrowing or the presence of osteophytes.
- Alignment of Phalanges: Ensure proper alignment of the phalanges. Malalignment may indicate joint instability or fractures.
- Sesamoid Bones: Sesamoid bones, particularly beneath the MCP joint of the thumb, should be visible. Evaluate their alignment and integrity.
By systematically assessing joint spaces and bony landmarks in a lateral finger X-ray, radiologists and healthcare professionals can identify pathological changes, guide treatment decisions, and contribute to an accurate diagnosis of conditions affecting the finger and hand.
Optimal Positioning for Special Views in Lateral Finger X-ray
Achieving accurate and diagnostic lateral finger X-rays often involves specific positioning techniques to highlight certain structures and provide a comprehensive view of the finger anatomy. Here’s a guide to the positioning for special views in lateral finger X-rays:
1. Oblique Views
Purpose: Oblique views help visualize specific aspects of the finger joint spaces and structures that may not be as clearly visible in a standard lateral view.
Positioning: Instruct the patient to position the affected finger at a 45-degree angle to the imaging receptor. Adjust the X-ray beam perpendicular to the finger, ensuring optimal penetration through the joint spaces.
2. Norgaard View (Lateral Oblique View of the Thumb)
Purpose: This specialized view is designed to assess the carpometacarpal (CMC) joint of the thumb.
Positioning: Position the thumb in a true lateral view with the palmar surface flat against the receptor. Angle the thumb at approximately 20 degrees, ensuring the metacarpal shaft is parallel to the receptor. Direct the X-ray beam perpendicular to the MCP joint.
3. Lateral Stress Views
Purpose: Lateral stress views are employed to evaluate joint stability and potential ligamentous injuries.
Positioning: Stabilize the finger in a lateral view with the joint in a neutral position. Apply stress by gently pulling or pushing on the finger, causing the joint to open or close. Image the finger during stress to assess joint stability.
4. Hyperextension Views
Purpose: Hyperextension views are useful for evaluating joint hypermobility or assessing specific ligamentous structures.
Positioning: Instruct the patient to hyperextend the affected finger while maintaining a lateral position. Ensure the X-ray beam is aligned perpendicular to the hyperextended joint.
5. Swimmer’s View (Lateral Oblique View of the Hand)
Purpose: This view is beneficial for assessing the entire hand, particularly the carpometacarpal (CMC) joint of the fifth digit.
Positioning: Position the hand in a true lateral view, ensuring the thumb is abducted. Angle the hand at approximately 45 degrees, allowing optimal visualization of the fifth CMC joint.
6. Lateral Thumb Projection
Purpose: This view is specialized for visualizing the lateral aspect of the thumb.
Positioning: Position the thumb in a true lateral view. Align the X-ray beam perpendicular to the thumb, focusing on the area of interest.
Ensuring proper patient cooperation and accurate positioning are essential for obtaining high-quality lateral finger X-rays, especially for special views. Collaborating with radiologic technologists and providing clear instructions to patients contribute to the success of obtaining specialized images for a comprehensive diagnostic evaluation.
Final Words
This guide aims to equip radiographers with the knowledge and skills required for optimal lateral finger X-ray imaging. By focusing on proper positioning, collimation, safety measures, and attention to detail, radiographers contribute significantly to accurate diagnostics and patient care in the assessment of finger conditions.