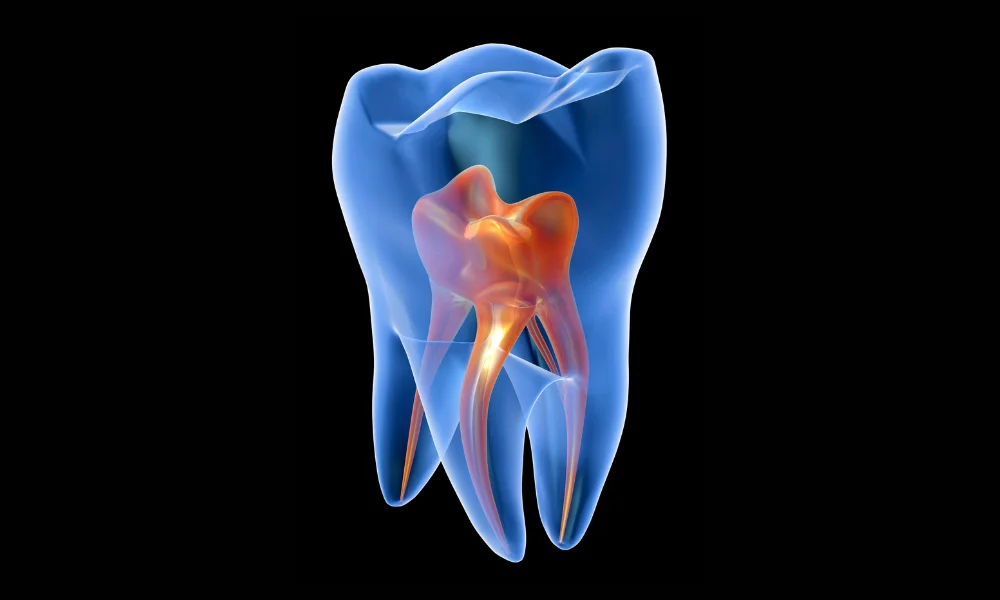
When it comes to root canal infections, the right diagnosis is the key to effective treatment. In this comprehensive blog, we’ll delve into the significance of X-rays of root canal infections in precisely diagnosing, exploring the process, benefits, and the crucial role they play in ensuring optimal oral health.
Table of Contents
Understanding Root Canal Infections
Root canal infections can be a source of discomfort and concern for many individuals. This section aims to provide a clear understanding of what root canal infections entail, exploring their causes, symptoms, and potential treatment options.
Causes of Root Canal Infections
Root canal infections typically originate from bacterial infiltration into the pulp of the tooth. Common causes include:
- Untreated Cavities: When cavities are left untreated, bacteria can penetrate the tooth, reaching the pulp.
- Tooth Trauma: Physical injuries to the tooth can create openings for bacteria to enter and cause an infection.
- Faulty Dental Procedures: Poorly performed dental procedures or inadequate fillings may leave room for bacterial entry.
Symptoms of Root Canal Infections
Recognizing the signs of a root canal infection is crucial for timely intervention. Symptoms may include:
- Severe Toothache: Persistent and intense pain in the affected tooth is a common indicator.
- Sensitivity to Hot or Cold: Discomfort when consuming hot or cold foods and beverages.
- Swollen Gums: Inflammation and tenderness in the surrounding gums.
- Pimple on the Gums: Formation of a pimple-like bump, known as a dental abscess, indicating infection.
Diagnosis and Treatment
Proper diagnosis involves dental examinations and imaging, often using X-rays. Once diagnosed, various treatment options are available:
- Root Canal Therapy: The infected pulp is removed, and the canal is cleaned, disinfected, and sealed.
- Apicoectomy: In cases of persistent infection, a surgical procedure to remove the apex of the tooth’s root may be necessary.
- Extraction: In severe cases, if the tooth cannot be saved, extraction might be recommended.
Preventing Root Canal Infections
Maintaining good oral hygiene is paramount in preventing root canal infections:
- Regular Dental Check-ups: Routine dental visits can help catch and address issues before they escalate.
- Timely Treatment: Addressing cavities and dental trauma promptly reduces the risk of infection.
- Proper Dental Care: Brushing, flossing, and using an antiseptic mouthwash contribute to overall oral health.
Understanding root canal infections empowers individuals to recognize symptoms early and seek timely dental care. With proper diagnosis and treatment, the discomfort associated with root canal infections can be alleviated, promoting oral health and overall well-being.
Also read: A Comprehensive Guide Through Root Canal X-rays
The Role of X-rays in Diagnosis
Penetrative Precision
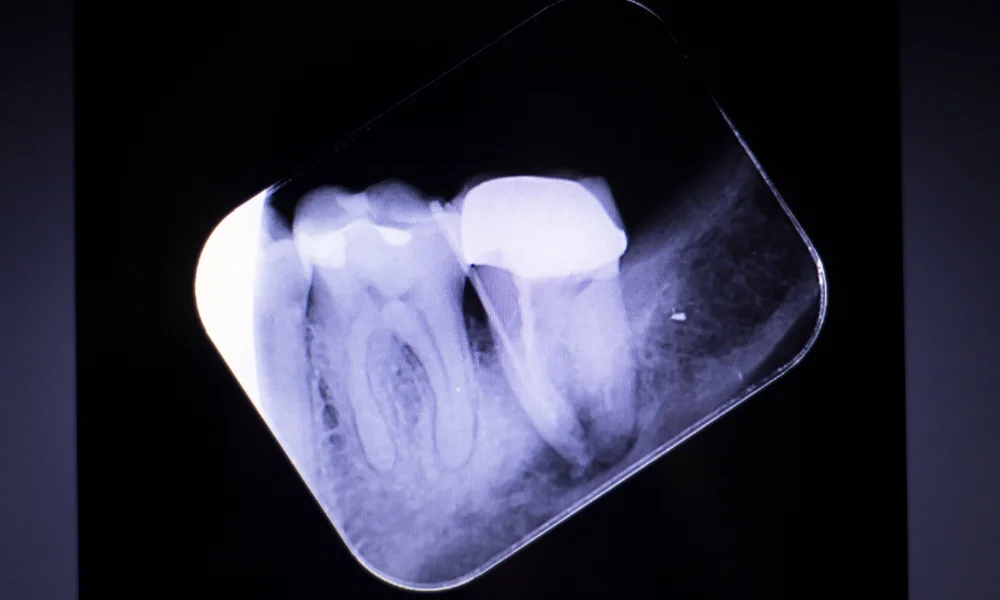
X-rays provide a detailed view of tooth structures, allowing dentists to identify infection sites, abscesses, and potential complications accurately.
Early Intervention
Detecting infections in their infancy enables prompt intervention, preventing the spread of bacteria and preserving the tooth.
Comprehensive Assessment
X-rays offer a comprehensive assessment of the tooth’s root, aiding dentists in planning precise and effective treatment strategies.
The X-ray Process
Patient Preparation
Patients are positioned for optimal X-ray capture, ensuring clear images without distortion. Protective measures like lead aprons minimize radiation exposure.
X-ray Machine Placement
Dentists strategically position the X-ray machine to capture images from various angles, providing a comprehensive view of the infected tooth.
Digital Advancements
Modern dentistry often utilizes digital X-rays, reducing radiation exposure and offering instantaneous, high-quality images for immediate analysis.
Benefits of X-ray Diagnosis
Accuracy in Identification
X-rays enable dentists to identify root canal infections accurately, distinguishing them from other dental issues with similar symptoms.
Treatment Customization
Precise diagnosis allows for tailored treatment plans, addressing the specific nature and extent of the root canal infection.
Monitoring Progress
X-rays aid in monitoring the progress of treatments, ensuring the elimination of infection and the success of interventions.
The Importance of Timely Diagnosis
Preventing Complications
Early detection prevents the escalation of infections, reducing the risk of complications such as abscess formation and damage to surrounding tissues.
Preserving Oral Health
Timely intervention preserves the affected tooth and surrounding structures, contributing to overall oral health and avoiding the need for extensive procedures.
Going Beyond Symptoms
Symptom Ambiguity
Root canal infections can manifest as various symptoms, making X-rays crucial for accurate diagnosis in cases where symptoms alone may be ambiguous.
Hidden Infections
Some infections may not exhibit noticeable symptoms, emphasizing the importance of X-rays in detecting hidden or asymptomatic infections.
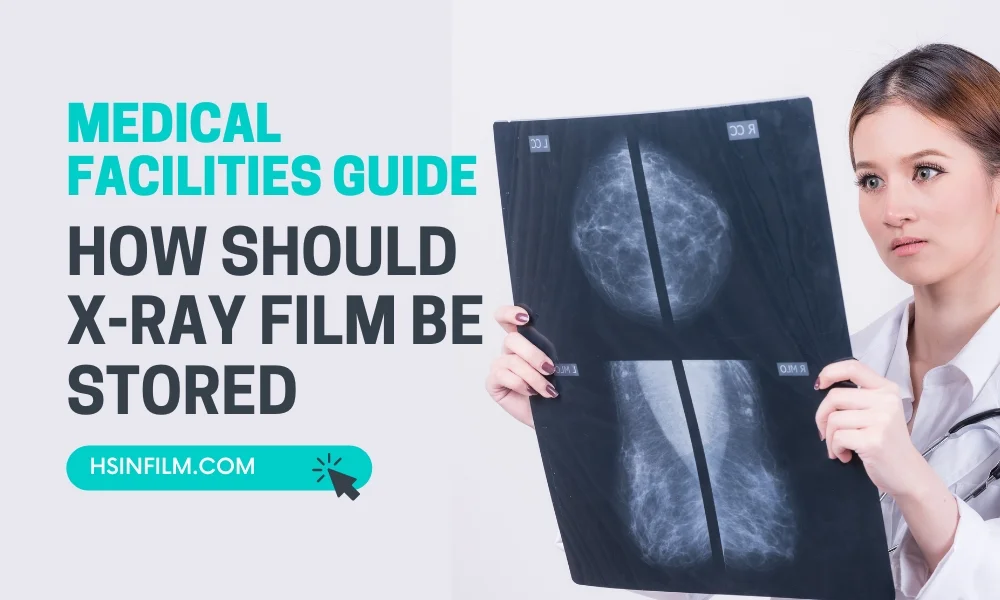
Unveiling Hidden Realities
When dealing with a root canal infection, a profound understanding goes beyond just addressing surface-level symptoms. The use of X-ray imaging emerges as a pivotal tool, allowing dental professionals to delve into concealed complexities and make informed decisions for comprehensive oral health.
Beyond the Surface
Root canal issues often hide beneath the visible symptoms, requiring a more in-depth exploration. X-ray images play a crucial role in providing a detailed analysis of tooth structures. They unveil hidden infections, showcase intricate canal anatomy, and highlight potential challenges that might not be immediately apparent during a routine examination.
How to Diagnose Patient from X-ray of Root Canal Infection?
Revealing the Unseen
Diagnosing a root canal infection requires a meticulous approach, and X-ray analysis stands as a crucial diagnostic ally. Beyond surface symptoms, these images unveil the unseen, providing an intricate view of the tooth’s interior.
Identifying Infections and Anatomy
X-rays highlight the presence and extent of infections, showcasing the affected areas within the root canal system. Moreover, they illuminate the intricate anatomy of the canals, helping dentists navigate complexities that may impact the treatment approach.
Precision in Treatment Planning
Armed with the insights gleaned from X-ray analysis, dentists can precisely plan the treatment. Whether it’s determining the extent of infection, locating additional canals, or assessing potential complications, this in-depth diagnosis sets the stage for a tailored and effective treatment strategy.
Enhancing Patient Care
The ability to diagnose root canal infections through X-ray analysis goes beyond detection; it enhances overall patient care. It allows for early intervention, reduces the risk of complications, and ensures that treatment is targeted, leading to more successful outcomes in managing and treating root canal infections.
Conclusion
In conclusion, X-rays are indispensable in the precise diagnosis of root canal infections. Their ability to reveal intricate details ensures early intervention, preventing complications and preserving overall oral health. Embrace the power of X-rays for a thorough understanding of your dental well-being.
Utilize HSIN Film’s Imaging Products for High-Quality Output
HSIN Film offers a range of cutting-edge imaging solutions for healthcare. From precise medical dry film to efficient thermal film, high-quality laser film, versatile inkjet printers, and rapid thermal printers, their products ensure accurate and reliable diagnostic imaging. With a commitment to precision and efficiency, HSIN Film empowers healthcare providers, contributing to the effectiveness of medical diagnostics and patient care.
Frequently Asked Questions (FAQ)
1. Why are X-rays important for diagnosing root canal infections?
X-rays provide detailed images of the tooth’s internal structure, helping to identify infections, assess the extent of damage, and plan treatment.
2. What signs of root canal infection can be detected on an X-ray?
X-rays can reveal signs such as dark spots indicating abscesses, widened periodontal ligament spaces, and bone loss around the tooth roots.
3. How does an X-ray help in planning root canal treatment?
X-rays help determine the number, shape, and length of root canals, and identify any complications, allowing for precise treatment planning.
4. What types of X-rays are used for diagnosing root canal infections?
Periapical X-rays and cone beam computed tomography (CBCT) scans are commonly used for detailed views of the tooth and surrounding bone.
5. Are X-rays safe for diagnosing root canal infections?
Yes, dental X-rays use low levels of radiation, and modern techniques and equipment further minimize exposure, making them safe for patients.
6. How often should X-rays be taken during root canal treatment?
X-rays are typically taken before, during, and after the procedure to monitor progress and ensure the infection is fully treated.
7. Can an X-ray detect all root canal infections?
While X-rays are highly effective, some infections might not be visible if they are very early or if there is significant bone density variation. Additional diagnostic methods may sometimes be needed.
8. What should I do if my X-ray shows a root canal infection?
Follow your dentist’s treatment plan, which may include a root canal procedure to clean and seal the infected tooth, and adhere to all follow-up care instructions.